Lindsay Hoshaw contributed to this post.
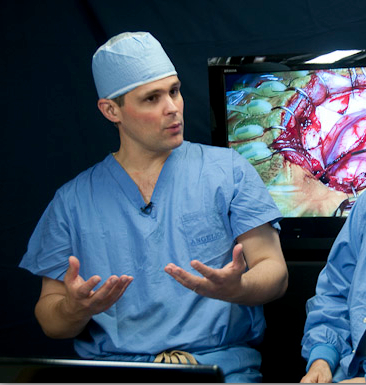
It’s 7 a.m. and neurosurgeon
Ed Smith, MD, is downing a Diet Coke as he reviews the MRIs of today’s patients. He sprints up a stairwell to greet his first patient in the pre-operating wing.
Thirteen-year-old Maribel Ramos, about to have brain surgery at Boston Children’s Hospital, sits in her bed fidgeting. Smith reassures her about the operation, promises they’ll shave off as little hair as possible, and gets Maribel to crack a smile by telling her he moonlights as a hairdresser.
Maribel’s operation is meant to correct a rare brain disorder called moyamoya—a narrowing of blood vessels that constrains blood flow in the brain. Smith becomes animated when he talks about it.
“Imagine the pipes in your bathtub don’t work and you’re only getting a trickle of water,” he explains. “But instead of fixing the pipes, you run a hose in through the window so you have a new source of water.”
Without surgery, moyamoya poses a five-year stroke risk of 60 to 90 percent. The operation, developed by Smith’s mentor, Michael Scott, MD, takes a healthy artery and attaches it to the part of the brain that isn’t getting enough blood. The artery naturally takes root, providing a permanent new source of blood.
Scott’s name got stuck in Smith’s head when he was just a teenager. “One of my best friends in high school, Seth, had a brain tumor,” Smith says as he walks out of pre-op. “He was treated at Boston Children’s, and although Seth ultimately passed away in college, the experience inspired me to become a neurosurgeon and work with Dr. Scott. It’s a joy to treat kids, because they can get better.”
Though he’s director of pediatric cerebrovascular surgery at Boston Children’s, Smith is the first to say that surgery isn’t always in a child’s best interest. He decides, for example, not to operate on a boy with a Chiari malformation, a condition where brain tissue protrudes into the spinal canal.
“I don’t have anything in my [surgical] toolbox that can make you better,” he tells the boy and his mom in the exam room.
Instead, Smith orders medication and schedules a follow-up MRI. “So tell me if you’ve heard this one,” Smith says to the boy. “A kid goes to his doctor with a carrot in his ears and a banana in his butt and peanut butter in his hair. And his doctor says, ‘Hmmm…you’re not eating right.’”
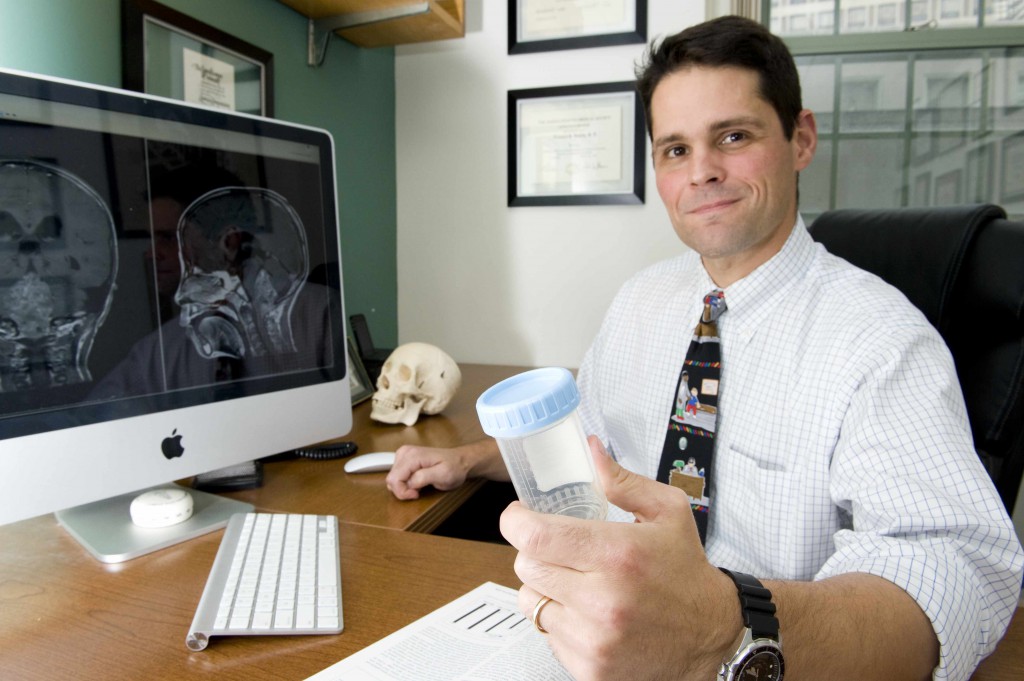
Peeing in a cup
In his laboratory across the street, Smith is looking for better ways to monitor his patients postoperatively—and determine whether he should even operate at all. Under the tutelage of another mentor, Marsha Moses, PhD, his sights are now on biomarkers—proteins whose presence may signal new or recurring brain disease.
Moses, director of the Vascular Biology Program, has pioneered the use of urine biomarkers to detect breast and ovarian cancer. Smith approached her after a lecture about a decade ago and soon found himself working in her lab. In 2008, he and Moses reported that a family of biomarkers Moses had identified—matrix metalloproteinases—are a good test for brain tumors.
“In my professional career, I’ve been fortunate to have Mike Scott as a sort of clinical ‘dad’ and Marsha Moses as a scientific ‘mom,’” Smith says.
Smith is now running a 12-hospital trial of a panel of urine biomarkers for monitoring pontine glioma or DIPG (diffuse infiltrative pontine glioma), a highly lethal brainstem tumor. He was able to incorporate the study into a larger treatment trial, hoping that the use of biomarkers will spare children from extra imaging tests and surgery.
“We can have people pee in a cup, drop it in a mailing box, and—hopefully—find out if their tumor has come back without us having to operate on them,” Smith says.
“Right now, if I take a tumor out of a child’s head, his parents are going to sweat bullets wanting to know if the tumor has grown back,” he adds. “They have to drive him to Boston every three months, pay for parking, walk over here, then see us knock the kid out with general anesthesia and do an MRI. Then we wake the kid up, send the family home and make them wait two or three days for a call after the radiologist reads the MRI. And often, I have to tell them, ‘Well, we’re not sure. Let’s check again in three months.’ And the parents are biting their nails for three months.”
Tumor recurrence may, in fact, show up in urine well before it’s visible on MRI. Smith also has data showing that urine markers can help to tell whether a child has moyamoya disease and, potentially, how well he’ll respond to surgery. He’s identified urine markers of arteriovenous malformations, and, in the future, hopes to find urine markers distinguishing between genetic subtypes of medulloblastoma. Right now, these subtypes—recently described by Neurologist-in-Chief Scott Pomeroy, MD, PhD, and collaborators at Dana-Farber/Children’s Hospital Cancer Center—can only be distinguished through tissue analysis.
Smith thrives on finding connections between his surgical practice and the findings of the lab scientists across the street, feeling they have a lot to teach each other.
“People in the lab may say, ‘We have this magic piece of RNA that we can kill tumor cells with,’ but they do it in a Petri dish or in a mouse,” he says. “And I may say, ‘You know what, to surgically put those agents in the brain is not feasible. You have to give an incredibly high dose; you have to reach parts of the brain that aren’t easily reachable. Let’s work on something else. Can we put this in some form of delivery that can be done with liquid? Is this something we can aim in a different direction?’”
Fixing the pipes
Two hours into Maribel’s operation, Smith locates an artery underneath her scalp that he can graft to her brain. “It’s amazing,” he marvels. “We’re in the part of her brain now that affects language and speech, and the part that makes Maribel, Maribel.”
After sewing the artery onto the surface of Maribel’s brain—the artery that should provide a new steady source of blood—Smith and his team carefully replace the small piece of her skull that they’d removed and stitch her skin back together. For Smith, it was a fairly “boring” operation—exactly what he’d hoped for—that should reduce Maribel’s stroke risk to just 4 percent in the next five years.
By 4 p.m., after a nine-hour day, Smith shows no signs of fatigue. He waxes passionate about his larger visions—to establish a multidisciplinary center for cerebrovascular neurosurgery, bringing together teams from Neurosurgery, Interventional Radiology and the Vascular Anomalies Center, and a fellowship that would give neurosurgeons protected time to do research.
“I’m a big fan of trying to make things happen—by taking advantage of all the great resources and smart folks at this hospital,” he says. Then he heads out the door for the gym.
Smith illustrates the moyamoya operation in this video:
Lindsey Hoshaw contributed to this post.