A picture may be worth a thousand words, but there’s something about holding an object in your hands that’s worth so much more. I realized this when John Meara, MD, DMD, handed me the skull of one of his patients.
A picture may be worth a thousand words, but there’s something about holding an object in your hands that’s worth so much more. I realized this when John Meara, MD, DMD, handed me the skull of one of his patients.
I turned it over in my hands while Meara, Boston Children’s Hospital’s plastic surgeon-in-chief, pointed out features like the cranium’s asymmetric shape and the face’s malformed left orbit.
Mind you, it wasn’t actually Meara’s patient’s skull in my hands. In reality, I was holding a high-resolution, plastic 3D model printed from the patient’s CT scans.
The printer that made that model—and several other models I saw in the last month—is the centerpiece of a new in-house 3D printing service being built by Peter Weinstock, MD, PhD, and Boston Children’s Simulator Program.
3D printing technology has exploded in the last few years, to the point where anyone can buy a 3D printer like the MakerBot for a couple of thousand dollars or order 3D printed products from services like Shapeways. Adobe even recently added 3D printing support to Photoshop.
And 3D printing is already making a mark on medicine. Full story »
(Ryan Somma/Flickr)
There’s no other way to say it: sepsis is a horrible disease. It typically starts with a runaway bacterial infection in the blood, followed by a runaway immune response that severely damages the body it’s trying to save. The results: shock, multiple organ failure and—in between 210,000 and 375,000 people in the United States alone every year—death.
Part of the problem is that the methods available for treating sepsis aren’t particularly good. Antibiotics can kill the bacteria, but that still leaves bacterial debris floating in the bloodstream, fueling the already over-excited inflammatory response.
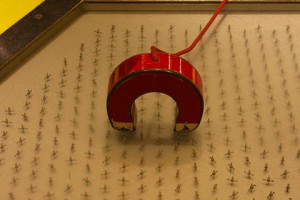
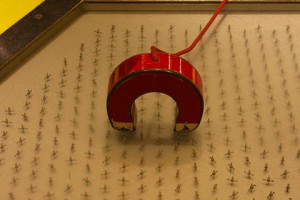
Removing the bacteria altogether—as fast as possible—would be the better solution. At least that’s what Daniel Kohane, MD, PhD, thinks. His lab at Boston Children’s Hospital’s Division of Critical Care Medicine has developed a new approach that combines magnetic nanoparticles, a synthetic molecule (called bis-Zn-DPA) that binds to the bacteria, and magnetized microfluidic devices to pull bacteria from the blood quickly and efficiently. Full story »
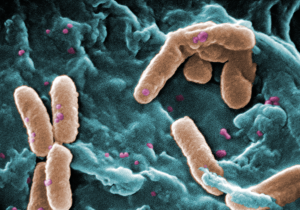
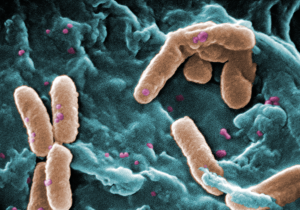
Bacteria like Pseudomonas aeruginosa (in brown) can move in on critically ill patients or those with cystic fibrosis. Could these bacteria hold the key to their own prevention? (CDC PHIL/Janice Haney Carr)
Putting children on a ventilator is sometimes necessary to save their lives, but it’s not without risks.
Doctors and nurses have to monitor ventilated patients carefully lest the machine over- or underinflate their lungs. Sometimes the very act of putting a child or adult on a ventilator can cause more lung damage (more on this in a future post). And life-threatening pathogens sometimes take advantage of a patient’s weakened state to set up shop in their lungs.
One of them is Pseudomonas aeruginosa, a bacterium long associated with hospital-acquired or healthcare-associated infections (sometimes also called nosocomial infections). Gregory Priebe, MD, and other researchers have spent 40 years trying to develop an effective vaccine against it.
“It’s often resistant to antibiotics, and can be very difficult to treat, even deadly,” says Priebe, a critical care specialist and infectious disease researcher at Boston Children’s Hospital. “People with cystic fibrosis (CF) also get lung infections with P. aeruginosa, where it can lead to a chronic and ultimately fatal infection.”
While there have been some limited successes in creating a vaccine, researchers have struggled to develop one that can work against multiple subtypes of the bug at the same time.
Priebe thinks he may have come up with a workaround—one that makes use of a little known arm of the immune system. Full story »
 A picture may be worth a thousand words, but there’s something about holding an object in your hands that’s worth so much more. I realized this when John Meara, MD, DMD, handed me the skull of one of his patients.
A picture may be worth a thousand words, but there’s something about holding an object in your hands that’s worth so much more. I realized this when John Meara, MD, DMD, handed me the skull of one of his patients.