Until this month, Agustín Cáceres’s baptism was the only time his family could come close to him. Everyone had to wear masks, gloves and gowns.
After that, he went into isolation, along with his mother Marcela, who came out only for meals. His father Alberto, and his four-year-old brother Jeremías, kept to a separate bedroom. Jeremías had to stop attending nursery school, for fear he’d bring home an infection his baby brother might catch. When Agustín’s relatives came to help out, they had to change their clothes and wash their hands, and couldn’t enter Agustín’s room.
Agustín, born in Argentina, has a form of X-linked Severe Combined Immunodeficiency, or SCID-X1, better known as “bubble boy disease.” It affects only boys, leaving their bone marrow unable to make T-lymphocytes, the white blood cells that fight infection.
The Cáceres’s first son had died from SCID-X1 at the age of 5 months. When Jeremías was born healthy, the family banked stem cells from his umbilical cord blood to benefit future siblings. But when Agustín was born, their tissue types turned out to be incompatible. Finding a matched donor was a daunting problem, and time was limited. Without intervention, Agustín was likely to die from a bacterial or viral infection before his first birthday.
Agustín’s immunologist in Buenos Aires, Matías Oleastro, heard of a clinical trial recruiting at Children’s Hospital Boston that was attempting to cure SCID-X1 with gene therapy. He had met Luigi Notarangelo and Sung-Yun Pai, the trial’s principal investigators at Children’s, at a medical conference.
Oleastro sent them a sample of Agustín’s blood, and Agustín was accepted as the first U.S. participant in the international trial, led by David Williams, chief of Hematology/Oncology at Children’s. “It was our best possibility,” said Marcela through a translator.
Agustín’s only other option was a bone marrow transplant from a partially matched donor, perhaps one of his parents. His chances could be improved by first giving him chemotherapy to kill the genetically defective cells in his bone marrow, but at the cost of highly toxic side effects. And with any bone marrow transplant, there’s a risk of graft-versus-host disease – the donor cells could launch a potentially fatal attack on Agustín himself.
The SCID-X gene therapy trial is one of several now in the pipeline. “The main advantage of gene therapy is that patients would receive their own cells, so there is no chance of graft-versus-host disease,” explained Pai, of Children’s Division of Hematology/Oncology. “There is also no time delay in finding a donor and no need for chemotherapy.”
Agustín arrived at Children’s last October with a mouth full of ulcers. He was admitted for 23 days to Children’s Hematopoietic Stem Cell Transplant Unit.
“We called a radio station in Jamaica Plain that plays tango music, and told our story,” Alberto said. “Someone heard our story and offered us a place to stay.” (Later, the family moved to a Ronald McDonald house.)
In December, Agustín underwent the gene therapy procedure. His bone marrow was extracted and purified and the blood stem cells manipulated in Dana Farber’s Connell and O’Reilly Families Cell Manipulation Core Facility (CMCF) to carry the new replacement gene. The gene was delivered by a specially engineered virus, known as a vector, that infects the cell without spreading in the body. A few days later, the treated cells were reinfused back into Agustín.
“We are fortunate to have the technical expertise of Dana-Farber’s CMCF and the superb nursing and clinical research staff of Children’s,” said Williams.
With luck, the treated cells would turn on the new gene, enabling them to make T-cells. When he arrived at Children’s, Agustín’s T-cell count was only 5, far too low to protect him. Over time, his doctors hoped, there would be enough healthy blood stem cells to make Agustín an ample supply of T-cells.
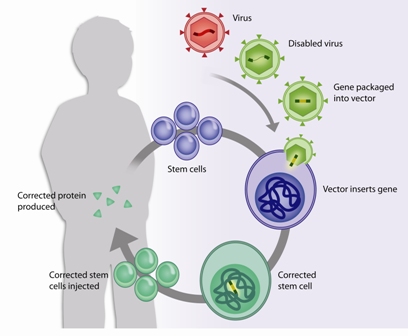
GENE THERAPY: The replacement gene was introduced into Agustín's blood stem cells by means of a vector, a genetically altered virus that enters cells without causing ongoing infection. The stem cells, corrected for the defect, were infused back into Agustín and are now creating normally functioning T-cells. (Click to enlarge.)
A week before his release in early May, a chubby Agustín, 10 months old, was full of smiles, sticking out his tongue and blowing bubbles. His T-cell count was up to about 170. “While this is not yet a normal number, he is producing more and more T lymphocytes,” said Notarangelo, of Children’s Division of Immunology, showing the family a graph. “It’s a steady and impressive increase – like a rocket. It should not take too long before he reaches a normal count.”
Agustín’s T cell function — completely absent last October — tested completely normal, and Pai’s lab demonstrated that the cells are able to produce the needed missing protein. Eventually, Agustín might also be able to produce antibodies, but for now he’ll need to keep receiving IV infusions of immunoglobulins every few weeks to guard against infection. Still, the gene therapy has been deemed a success so far.
“He has gained weight, and all of his organs are functioning normally,” Notarangelo told the family as he examined Agustín. “His muscle tone and behavior are appropriate for his age. Basically he is a healthy child.”
The Cáceres family is now back in Argentina – flying back with no special precautions on the airplane. Oleastro will see Agustín weekly, conduct frequent clinical and laboratory exams – with research blood samples shipped to Boston — and stay in close contact with Children’s. They made this video to thank the Children’s-DFCI staff:
If all goes well, Agustín won’t need to return to Boston until a year from now, but he’ll need to be closely monitored until he is 15 years old. The first trials of gene therapy for SCID-X1, in Paris and London, reported leukemia as a serious side effect. This set the field back, but led to an international effort to find the culprit – the gene-delivery vector – and improve it by removing the cancer-triggering elements and powering down the level of expression of the SCID-X1 gene.
Although laboratory studies in cells and experiments in animals show the newly designed vector to be safe, the team is being extra-cautious. “Many people are watching us,” says Notarangelo. “A lot of eyes are on this trial.”