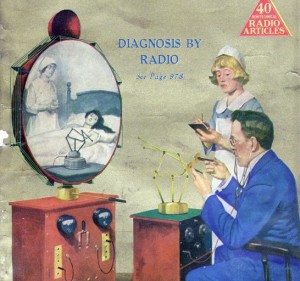
Back in the 1920s, when medicine was more an art than a science and doctors made home visits, a publishing and radio pioneer named Hugo Gernsback predicted the future of telehealth. As described on Smithsonian.com, he wrote of a device called the TeleDactyl: “a future instrument by which it will be possible for us to ‘feel at a distance’”—dactyl, from the Greek, meaning finger.
Since that time, the practice of medicine has changed dramatically. Our understanding of the human body has advanced beyond our wildest dreams, producing drugs, devices and procedures that have made hospitals a place for healing and curing. At the same time, home visits were abandoned in favor of the office visit, making doctors more efficient. Almost 100 years later, several converging forces are making the home visit popular again, increasing the likelihood of seeing Gernsback’s vision become a reality.
The rollout of the Affordable Care Act, which will add millions of new patients to the health care system, comes at the same time that we have a shortage of primary care doctors, specialists and other care providers. In addition, physicians and hospitals are being urged to innovate around care delivery in response to new care models (accountable care organizations, patient-centered medical homes and alterative payment models). These arrangements put them at financial risk—but also give them shared savings opportunities.
At the same time, technology-savvy and social-media-hungry Millennials and Gen X consumers, armed with relatively inexpensive smartphones, tablets and unlimited Internet access, have become profoundly engaged in their own health, downloading apps and buying peripherals. Devices like JawBone Up and Scanadu Scout, as well as smartclothes like the smart “onesie” from Mimo or a shirt from OMSignal, quantify and track every possible bodily function and activity, including blood glucose levels, calories consumed, heart rate, body temperature, miles walked and quality of sleep.
All of these forces are prodding health care organizations of all shapes and sizes to develop a strategy for delivering care to the Facebook/Twitter/Instagram /SnapChat generation of patients wherever and whenever they want it.
And that has poised telehealth for massive growth. Health systems, hospitals, physician groups and others are combining in new ways to offer virtual visits to their patients. Companies like American Well, Teladoc, MDLive and RingMD are findings traction by leveraging web technologies that enable patients and clinicians to communicate securely via text, email, chat, phone or video at a time and place of their choosing. Large electronic medical record companies like Cerner and EPIC are beginning to incorporate these features into their own products. And health insurance companies (Aetna, Wellpoint, Cigna, Highmark and others) are jumping on the bandwagon.
It makes sense. Reports suggest that patients and families using telemedicine are very satisfied with the convenience and the timeliness of the care. Insurers that reimburse for virtual telehealth visits, and providers that have assumed financial risk, can avoid costly but potentially unnecessary ER visits, or prevent rehospitalizations by monitoring recently discharged patients. And employers can reduce worker absenteeism and improve productivity by offering telehealth visits as a benefit to their employees.
So we have come back to what we thought was a bygone era. The home visit has returned—albeit with a 21st century twist—and I expect it will make up a rapidly increasing percentage of total outpatient visits this year. The technology also will accelerate, as evidenced by the American Telemedicine Association’s partnership with X-Prize, a contest to develop a Star Trek “tricorder-like” handheld device that can diagnose 15 different conditions and capture five vital biometrics.
By the year 2020, I expect to see clinicians remotely palpate a patient’s abdomen or manipulate a patient’s knee joint and receive tactile feedback on the far end—finally realizing the dream of the TeleDactyl.