The TeleDactyl, as depicted on the cover of Science and Invention magazine in 1925.
Shawn Farrell, MBA, is Telemedicine and Telehealth Program Manager at Boston Children’s Hospital.
Back in the 1920s, when medicine was more an art than a science and doctors made home visits, a publishing and radio pioneer named Hugo Gernsback predicted the future of telehealth. As described on Smithsonian.com, he wrote of a device called the TeleDactyl: “a future instrument by which it will be possible for us to ‘feel at a distance’”—dactyl, from the Greek, meaning finger.
Since that time, the practice of medicine has changed dramatically. Our understanding of the human body has advanced beyond our wildest dreams, producing drugs, devices and procedures that have made hospitals a place for healing and curing. At the same time, home visits were abandoned in favor of the office visit, making doctors more efficient. Almost 100 years later, several converging forces are making the home visit popular again, increasing the likelihood of seeing Gernsback’s vision become a reality.
The rollout of the Affordable Care Act, which will add millions of new patients to the health care system, comes at the same time that we have a shortage of primary care doctors, specialists and other care providers. Full story »
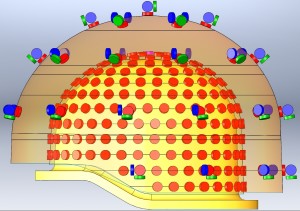
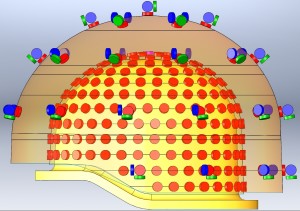
This array of sensors surrounding a baby's head will give researchers and eventually clinicians a high-resolution image of neural activity.
Imagine you’re a clinician or researcher and you want to find the source of a newborn’s seizures. Imagine being able to record, in real time, the neural activity in his brain and to overlay that information directly onto an MRI scan of his brain. When an abnormal electrical discharge triggered a seizure, you’d be able to see exactly where in the brain it originated.
For years, that kind of thinking has been the domain of dreams. Little is known about infant brains, largely because sophisticated neuroimaging technology simply hasn’t been designed with infants in mind. Boston Children’s Hospital’s Ellen Grant, MD, and Yoshio Okada, PhD, are preparing to launch a new magnetoencephalography (MEG) system that will soon turn those dreams into reality. Full story »
 2013 saw an accelerated crumbling of borders and boundaries in health care, fueled by technological and scientific advances. Boundaries between high-tech Western medicine and global health practices have begun blurring in interesting ways, as are those between home and hospital, patient and doctor and even a patient’s own body and the treatment used for her disease.
2013 saw an accelerated crumbling of borders and boundaries in health care, fueled by technological and scientific advances. Boundaries between high-tech Western medicine and global health practices have begun blurring in interesting ways, as are those between home and hospital, patient and doctor and even a patient’s own body and the treatment used for her disease.
Last year also saw a fierce political fight over the Affordable Care Act (ACA)—aka Obamacare—ending in some six million people crossing the boundary from uninsured to insured, according to HMS, if you count Medicaid and Children’s Health Insurance Program eligibles.
What does all this portend for 2014? This year, Vector asked leaders from all walks of life at Boston Children’s Hospital to weigh in with their predictions. Full story »
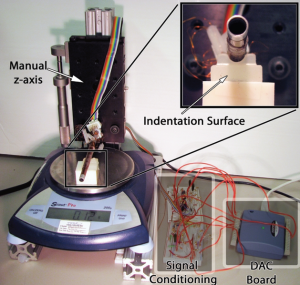
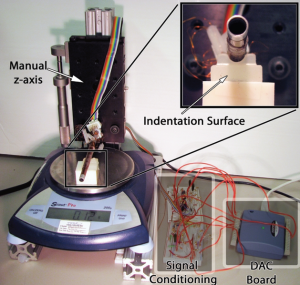
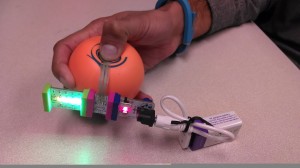
Experimental setup for calibrating the sensing skin. Each sensor pad is lowered onto the indentation surface placed on a weight-measuring scale. Changes in the channel resistance are processed through analog signal conditioning and a DAC board, and recorded on a computer. (Images: J Neurosurgery: Pediatrics)
When surgeons perform image-guided minimally invasive procedures using an endoscope, some aspects of visualization and image quality are typically compromised as compared with open surgeries in which the physician can peer into the body. However, a new pressure-sensing material, placed over an endoscope, may someday provide surgeons with additional guidance and protect healthy tissue during these procedures.
“Neurosurgeons, especially pediatric neurosurgeons, are increasingly using neuroendoscopy to perform minimally invasive brain and spine surgery,” notes Patrick Codd, MD, from the Department of Neurosurgery at Boston Children’s Hospital, who was the lead author on a study evaluating this new material.
“Whenever you move to image-guided minimally invasive surgery, there is typically a tradeoff between the resolution of the image and the field of view,” where you have one but not the other, says Pierre Dupont, PhD, chief of Pediatric Cardiac Bioengineering at Boston Children’s and senior author on the study. Full story »
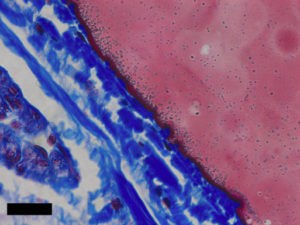
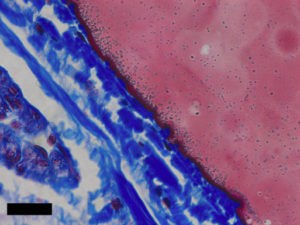
A close-up view of the adhesive (pink) interacting with collagen tissue (blue). Images courtesy Karp Lab.
A safe and effective adhesive, or glue, that can be used internally in the body has been a pressing need in medicine. Its creation has faced major hurdles—not the least of which is ensuring the glue is nontoxic and capable of repelling fluids—but a new study published today in
Science Translational Medicine offers a potential breakthrough.
Congenital heart defects occur in nearly 1 in 100 births, and those that require treatment are plagued with multiple surgeries to deliver or replace implants that do not grow along with the child. Currently, therapies are invasive and challenging due to an inability to quickly and safely secure devices inside the heart. Sutures take too much time to stitch and can cause stress on fragile heart tissue, and the available clinical adhesives are subpar.
“Current glues are either toxic or easily washout in the presence of blood or react immediately upon contacting water,” says Pedro del Nido, MD, chief of Cardiac Surgery at Boston Children’s Hospital and senior co-author of the study. “The available options also tend to lose their sticking power in the presence of blood or under dynamic conditions, such as in a beating heart.” Full story »
 Scaffolds made of silk could give doctors a simple, more effective material for performing bladder augmentation in people with urinary tract defects—to relieve incontinence and prevent kidney damage in children born with small bladders, for example. Rather than using cells to augment the bladder, a complicated process, silk could provide an “off the shelf” option, says Carlos Estrada, MD, a urologist at Boston Children’s Hospital.
Scaffolds made of silk could give doctors a simple, more effective material for performing bladder augmentation in people with urinary tract defects—to relieve incontinence and prevent kidney damage in children born with small bladders, for example. Rather than using cells to augment the bladder, a complicated process, silk could provide an “off the shelf” option, says Carlos Estrada, MD, a urologist at Boston Children’s Hospital.
Recent research by Estrada and Joshua Mauney, PhD, shows that scaffolds made of fibroin (the protein that makes up raw silk) have worked well in augmenting bladders in animal models—without the need for cells.
Estrada and Mauney built on the work of Anthony Atala, MD, who became head of the Institute for Regenerative Medicine at Wake Forest after undertaking pioneer work in tissue engineering in Boston Children’s Urology Department. Full story »
 Assisted by a congressional mandate, the FDA has taken a new approach to helping clinical innovators overcome barriers to moving pediatric medical devices from the research stage to commercialization. So says Linda Ulrich, MD, director of the Pediatric Device Consortia Grant Program at the FDA’s Office of Orphan Products Development, who recently spoke at an Innovators’ Forum cosponsored by her office and Boston Children’s Hospital’s Innovation Acceleration Program.
Assisted by a congressional mandate, the FDA has taken a new approach to helping clinical innovators overcome barriers to moving pediatric medical devices from the research stage to commercialization. So says Linda Ulrich, MD, director of the Pediatric Device Consortia Grant Program at the FDA’s Office of Orphan Products Development, who recently spoke at an Innovators’ Forum cosponsored by her office and Boston Children’s Hospital’s Innovation Acceleration Program.
Regulation and reimbursement are the largest barriers to medical device innovation. “The time it takes to develop a medical device and get it to the U.S. market can take a range from 18 months to 10 years,” says Ulrich.
The stages of device development are concept, prototype, preclinical and clinical testing, manufacturing and marketing—only for the device to become obsolete within as little as 18 months after commercialization. Inventors need to consider the return on investment after their products receive regulatory approval, given the time and funding it takes to get them to market, says Ulrich. Full story »
 Michael Docktor, MD, is a pediatric gastroenterologist, director of clinical mobile solutions at Boston Children’s Hospital and a co-founder of Hacking Pediatrics. Above: The Hacking Pediatrics executive team: Judy Wang, MS; Michael Docktor, MD; Alex Pelletier, MBA; Margaret McCabe, PhD, RN, PNP; Kate Donovan, PhDc, MBA, BS, from Boston Children’s Hospital. (Photos: K.C. Cohen)
Michael Docktor, MD, is a pediatric gastroenterologist, director of clinical mobile solutions at Boston Children’s Hospital and a co-founder of Hacking Pediatrics. Above: The Hacking Pediatrics executive team: Judy Wang, MS; Michael Docktor, MD; Alex Pelletier, MBA; Margaret McCabe, PhD, RN, PNP; Kate Donovan, PhDc, MBA, BS, from Boston Children’s Hospital. (Photos: K.C. Cohen)
A hackathon is most easily explained by relating it to the crowd-sourced, time-crunched challenges that we see every day in pop culture. From “Top Chef” to “The Apprentice” to “Extreme Makeover,” television is teeming with passionate individuals trying to solve a difficult task with incredibly constrained resources and time. What results is often remarkable by any standard and speaks to the power of concentrated, collaborative problem solving.
When the challenge involves children and their health, the results can be magical, as witnessed by the weekend-long Hacking Pediatrics in late October, the first event of its kind. More than 150 “hackers,” including engineers, designers, software developers, entrepreneurs and roughly 40 clinicians gathered to create ground-breaking solutions for children and their families. Full story »

A 4.2-lb baby girl in the new 1.5 Tesla MRI magnet, designed for use in the NICU. (Images courtesy of Cincinnati Children’s Hospital Medical Center)
Charles Dumoulin, PhD, is the director of the Imaging Research Center at Cincinnati Children’s Hospital Medical Center (CCHMC) and a professor of pediatric radiology at University of Cincinnati College of Medicine. He led the team of scientists and engineers from CCHMC’s Imaging Research Center who won the Clinical Innovation Award at Boston Children’s Hospital’s National Innovation Pediatric Summit + Awards in September.
Experience suggests that magnetic resonance imaging (MRI) and advanced MR techniques such as spectroscopy and diffusion imaging offer substantial benefits when diagnosing problems in premature babies. However, today’s MR systems poses significant logistical barriers to imaging these infants. We have been working to change that.
MRI provides an unparalleled ability to visualize anatomy without the hazards of ionizing radiation. Yet premature and sick babies in neonatal intensive care units (NICUs) are usually too delicate to leave the unit. The few babies who receive MRI today must be accompanied by NICU staff during transport to and from the Radiology Department. This process is often a multi-hour ordeal and reduces the staff available to care for other babies in the NICU. Moreover, infants must be imaged in an adult-sized MRI scanner Full story »
 Israel Green-Hopkins, MD, is a second-year fellow in Pediatric Emergency Medicine at Boston Children’s Hospital and a fierce advocate for innovation in health information technology, with a passion for design, mobile health, remote monitoring and more. Follow him on Twitter @israel_md.
Israel Green-Hopkins, MD, is a second-year fellow in Pediatric Emergency Medicine at Boston Children’s Hospital and a fierce advocate for innovation in health information technology, with a passion for design, mobile health, remote monitoring and more. Follow him on Twitter @israel_md.
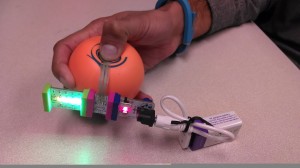
At the Hacking Pediatrics event in late October, I was fortunate to collaborate with a team interested, like I am, in patient engagement. After the initial idea-pitching phase of the hackathon, where clinicians present unsolved problems to an audience of techies and entrepreneurs, I joined a group of nearly 15 hackers who felt our desires to be similar. The prototype at left was our end result, but we had no idea then where our interest would lead.
At the beginning, in fact, our greatest challenge was determining exactly what problem we would try to solve. Full story »