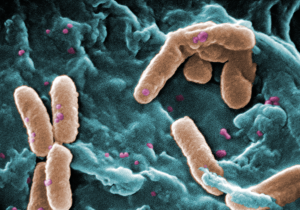
Bacteria like Pseudomonas aeruginosa (in brown) can move in on critically ill patients or those with cystic fibrosis. Could these bacteria hold the key to their own prevention? (CDC PHIL/Janice Haney Carr)
Putting children on a ventilator is sometimes necessary to save their lives, but it’s not without risks.
Doctors and nurses have to monitor ventilated patients carefully lest the machine over- or underinflate their lungs. Sometimes the very act of putting a child or adult on a ventilator can cause more lung damage (more on this in a future post). And life-threatening pathogens sometimes take advantage of a patient’s weakened state to set up shop in their lungs.
One of them is Pseudomonas aeruginosa, a bacterium long associated with hospital-acquired or healthcare-associated infections (sometimes also called nosocomial infections). Gregory Priebe, MD, and other researchers have spent 40 years trying to develop an effective vaccine against it.
“It’s often resistant to antibiotics, and can be very difficult to treat, even deadly,” says Priebe, a critical care specialist and infectious disease researcher at Boston Children’s Hospital. “People with cystic fibrosis (CF) also get lung infections with P. aeruginosa, where it can lead to a chronic and ultimately fatal infection.”
While there have been some limited successes in creating a vaccine, researchers have struggled to develop one that can work against multiple subtypes of the bug at the same time.
Priebe thinks he may have come up with a workaround—one that makes use of a little known arm of the immune system.
Neutrophils (with purple blobs) could be powerful allies against P. aeruginosa infections. (Dr. Graham Beards/Wikimedia Commons)
Most vaccines try to teach the body to produce proteins called antibodies when it sees a particular pathogen. But because the immune system can have a hard time making effective antibodies against P. aeruginosa, Priebe wanted to take a different tack. “We wanted to build a vaccine that convinces the immune system to turn on a kind of immune response called Th17 immunity.”
In this form of immunity, the body reacts to a pathogen not by producing antibodies, but by turning on a kind of immune cell called a neutrophil. The neutrophils then take on the role of hunting down and clearing the bacteria from the body.
Priebe and his colleagues had already made a vaccine made from weakened P. aeruginosa bacteria that can weakly activate the Th17 pathway. They wanted to make a vaccine that activates it strongly, yet avoid the potential side effects of vaccines made from weakened bacteria (such as inflammation and infection).
To do that, Priebe and his colleagues (including researchers down the street at Harvard Medical School and at Brigham and Women’s Hospital) used mouse cells to screen a library of potential P. aeruginosa antigens (parts of a pathogen that get the immune system’s attention), looking for ones that trigger a Th17 response.
As Priebe’s team recently revealed in the American Journal of Respiratory and Critical Care Medicine, five antigens fit the bill, one of which seemed particularly promising. It’s called PopB, and is itself part of the reason why P. aeruginosa is so dangerous. To wreak its own particular brand of havoc, P. aeruginosa injects a toxin into cells using a needle built from its own proteins; PopB is one of those proteins.
P. aeruginosa uses what's essentially a microbial needle to do its dirty work. But a part of that needle might also make a good vaccine target. (Pixie/Wikimedia Commons)
“When we immunized mice with PopB, we saw that it protected them from P. aeruginosa pneumonia,” he says. “And it did so by activating Th17 immunity and pulling in neutrophils, just as we’d hoped.”
Whether the vaccine will work in people remains to be seen; Priebe’s team is gearing up to run those studies. But he’s hopeful, and sees a lot of utility for the vaccine should it be successful.
“We’d probably initially focus on groups of people who, because of their jobs, are at high risk of ending up on a ventilator, including soldiers, firemen and police,” he says. “We also hope eventually to test it in people with CF but will need first to be sure it doesn’t worsen their lung inflammation.
“Vaccination is just one strategy for stopping P. aeruginosa,” Priebe notes. “We’re also working on better infection control procedures so that we can stop it from moving into patients or from patient to patient within a hospital setting. An effective vaccine, though, would be an excellent tool to have in our kit.”







