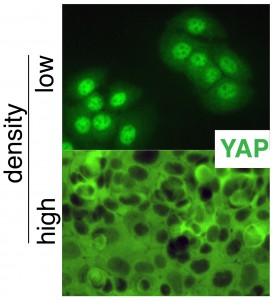
GROWTH CONTROL: Under conditions of low cell density (top image), Yap1, shown in green, is concentrated in cell nuclei, where it turns on growth-promoting genes. Under conditions of cell crowding (bottom image), Yap1 is kept out of cell nuclei (black areas) and is unable to act. Instead it's spread throughout the cell cytoplasm.
Generating new skin for burn victims and treating skin cancer are two sides of the same coin, according to a new study, which also reveals an inborn “crowd control” mechanism that flips the coin. Healthy people have a switch that senses how tightly cells are packed in the “neighborhood,” and turns growth-promoting genes on or off as needed in epidermal (skin-forming) stem cells.
Fernando Camargo, a researcher in the Children’s Hospital Boston Stem Cell Program, has worked out how this switch works and why it’s stuck “on” in cancers like squamous cell carcinoma, the second most common skin cancer. That could be a fresh clue to treating these cancers.
And as Camargo’s team demonstrated in mice, tinkering with that same switch could grow new skin when it’s needed, to heal a burn or ulcer.
Camargo, born in Peru and named a Pew Scholar last year at the age of 33, has been interested in understanding what maintains organs at a specific size. How do our skin and kidneys and livers “know” when it’s time to stop growing?
The answer is a great example of mechanobiology – the interface of biology and engineering. “Our work shows for the first time a direct link between environmental signaling cues, such as cell density, and a transcriptional regulator involved in organ size,” says Camargo.
The story began several years ago with the discovery of a size-control pathway known as Hippo – so named because its inactivation in fruit flies (in which it was initially discovered) led to growth of enormous tumors, oversized eyes and wings eight times normal size. Larger animals with defects in this organ-size widget also have overgrown body parts.
A key regulator of Hippo is a molecule called Yap1 – found not just in fruit flies but in mammals, including humans. Earlier, Camargo showed that manipulation of Yap1 in the mouse liver can increases the organ’s size by four-fold.
Camargo’s team now demonstrates that Yap1 regulates proliferation of epidermal stem cells, and that it’s controlled by a second molecule known as alpha-catenin, a tiny sensor that imparts information on the surrounding cell density.
When skin cells are densely packed, alpha-catenin inactivates Yap1, keeping it out of the cell nucleus and preventing it from triggering any more cell growth. Which is as it should be. When density goes down, this brake is disabled, so Yap1 is free to enter the nucleus and turn on genes that stimulate proliferation of skin cells. Also as it should be.
But alpha-catenin is known to be inappropriately silenced in skin and other epithelial cancers, such as colon cancer, so the “stop growing” message never gets sent, or is never heeded. “By activating alpha catenin, or by directly inhibiting Yap1, we could try to suppress tumor growth,” Camargo says.
On the other side of the coin, Yap1 could be manipulated to grow more skin when you want it. “The more Yap1 you have in your stem cells, the thicker your skin grows,” says Camargo, also a member of the Harvard Stem Cell Institute. “If you don’t have this molecule, the skin fails to expand. The stem cells cannot keep up.”
Now that this “switch” for skin growth is known, manipulating it could provide ways to grow skin cells when they’re needed or, conversely, to stop cancer growth. Camargo’s team is conducting screening tests to find small molecules that mimic Yap1, to improve skin regeneration at the site of a wound, or that inhibit Yap1 to treat skin tumors.






