 Israel Green-Hopkins, MD, is a second-year fellow in Pediatric Emergency Medicine at Boston Children’s Hospital and a fierce advocate for innovation in health information technology, with a passion for design, mobile health, remote monitoring and more. Follow him on Twitter @israel_md.
Israel Green-Hopkins, MD, is a second-year fellow in Pediatric Emergency Medicine at Boston Children’s Hospital and a fierce advocate for innovation in health information technology, with a passion for design, mobile health, remote monitoring and more. Follow him on Twitter @israel_md.
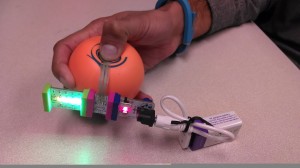
At the Hacking Pediatrics event in late October, I was fortunate to collaborate with a team interested, like I am, in patient engagement. After the initial idea-pitching phase of the hackathon, where clinicians present unsolved problems to an audience of techies and entrepreneurs, I joined a group of nearly 15 hackers who felt our desires to be similar. The prototype at left was our end result, but we had no idea then where our interest would lead.
At the beginning, in fact, our greatest challenge was determining exactly what problem we would try to solve. We flexed through multiple ideas: from patient education platforms to an app that would help clinicians measure pain on a scale to video tutorials for disease management. It was not until 18 hours before the deadline that we “pivoted” for the last time. One group set out to build a pain app; the other team, which I joined, tried to understand the problem of pain assessment in kids.
In business development, a “pivot”—a term for course correction popularized by Eric Ries’s influential book, “The Lean Startup”—is traditionally considered a last-ditch effort in the face of a failing trajectory. In pivoting, some groups lose their bearing entirely, as their creative energy dissipates rather than getting channeled into a problem-focused solution.
Now back at square one, our smaller team homed in a specific problem: How might we empower pediatric patients to more effectively communicate their pain and receive more effective, personalized treatment?
Our team was diverse and energized: Jon Scannell, RN, a nurse from the Orthopedic Center at Boston Children’s Hospital; Kelsey Bassanini, RCIS, a biomedical engineer and cardiovascular invasive specialist; Andrew Brown, MD, a radiology resident at University of Toronto and an MIT Sloan MBA student; Mahek Shah, MD, a physician-entrepreneur and seasoned hacker; Samantha Dempsey, a talented graphic designer from the Rhode Island School of Design; and myself.
Mahek and Andrew, our business specialists, evaluated the scope of the problem of pain communication and pain assessment in pediatrics. Jon, with first-hand clinical experience assessing pain, led discussions with live patients—some of them attending the hackathon, others visited later on the floors of Boston Children’s—to find out why communicating pain is so challenging.
This research, while brief and limited, identified a primary issue: Patients lack a truly engaging medium to communicate their pain.
For clinicians, validated pain measurement involves administering standardized pain scales, where 10 is the most pain and 1 the least, or a similar scale for younger children with pictures of faces. But in our ideation process, we realized that for children, a familiar physical item to interact with might reveal their pain in a self-directed way. Might such a “de-medicalized” tool make children more willing and able to express pain? Could it become something they expect and rely on for pain communication?
Working through the evening and early morning hours, team members proposed different ideas—an animal to hug? A light that responds to touch? We finally settled on a ball: one that makes a noise when squeezed while illuminating a scale of lights based on the intensity of the squeeze. The next question, of course, was how.
 Our design for The Comfy Ball won Best Hardware Hack, but it was only a beginning. Our team continues to meet weekly to pinpoint how and when a child might use the ball to convey pain. Do they squeeze it when they feel pain, or in response to a question about their pain? Should it have connectivity to an app? As we develop use cases for The Comfy Ball in acute and chronic pain, we feel pain communication in pediatrics is bound to be transformed for the better.
Our design for The Comfy Ball won Best Hardware Hack, but it was only a beginning. Our team continues to meet weekly to pinpoint how and when a child might use the ball to convey pain. Do they squeeze it when they feel pain, or in response to a question about their pain? Should it have connectivity to an app? As we develop use cases for The Comfy Ball in acute and chronic pain, we feel pain communication in pediatrics is bound to be transformed for the better.
People often grade and critique the “success” of hackathons, judging the scalability of the ideas, the continuation of projects over time and the dead ends. For me, having witnessed countless failed attempts to solve numerous health care problems, the story of The Comfy Ball stands out. Watching patients, parents, clinicians, engineers and designers collaborate to drive solutions is a unique experience—one I’d like to see diffuse seamlessly through health care.







