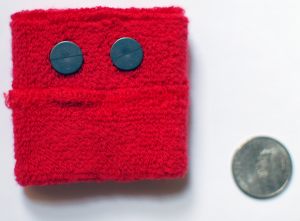
This comfy wristband can sound an alarm when a child is having a seizure, and can help doctors better time medication dosing.
This is the first post in a series about new approaches for seizures and epilepsy.
Seizures are often hard to track in children with epilepsy, making it difficult for doctors to optimize their treatment. For parents, the greatest worry is that their child will have a life-threatening seizure in the middle of the night or away from home, unable to get help. And what about when that child goes off to college?
“Every parent asks, ‘What can I do to prevent my child from harm?’” says Tobias Loddenkemper, MD, a neurologist in the Epilepsy Program at Boston Children’s Hospital.
Loddenkemper also wanted to better understand his patients’ seizure patterns so he could better time the dosing of their medications. He’s been testing a wristband sensor system, developed by Rosalind Picard, ScD, and colleagues at the MIT Media Lab (Epilepsia, March 20), and thinks it could be part of the solution.
The wristband carries two kinds of sensors: One, a motion detector, used in some iPhones to detect tilts and shakes, detects the repetitive movements of a convulsion. The other, a skin conductance measurer like those used in lie detectors, is sensitive to tiny amounts of sweat, indicating activation of the sympathetic nervous system. Combining this information, the system could be programmed to sound an alarm when a predetermined threshold is reached.
Picard developed the wristband to get objective physiologic measures of emotional states, such as anticipating meltdowns in autistic children. At the time, a graduate student in her lab, Miriam Madsen, was also doing research at Boston Children’s, and connected Picard with her father, Joseph Madsen, MD, a neurosurgeon at the hospital. The two institutions began collaborating, studying the relationships between wristband indicators of emotion and brain signals from children with epilepsy.
The hospital’s Long Term Epilepsy Monitoring Unit, where patients are tracked with EEGs for up to a week to find the source of their seizures in the brain, offered an ideal setting to try out the sensors: Information from the children’s EEG tracings could be readily compared with information from the wristband. Loddenkemper took an interest in the project, and began working with Ming-Zher Poh in Picard’s lab.
During the course of their study, 80 children wore the wristband during EEG monitoring. The EEGs documented 16 generalized tonic-clonic seizures (full-blown seizures involving stiffening and shaking of the body and loss of consciousness, also known as grand mal seizures) in seven children. Fifteen of the 16 were also detected by the wristband.
The other 73 patients never had a seizure. Over the course of some 3,500 monitoring hours, their wristbands sounded a total of 102 false alarms, occurring at least once in about a third of the children. (Four children accounted for a large number of them — through dice-throwing, gaming on the Nintendo Wii or hand flapping, common in developmental delay and autism). Loddenkemper believes these false alarms will diminish as the systems get “trained” with more and more data; eventually, the wristband could be taught to recognize what seizures look like in different individuals.
In the future, the wristband could potentially transmit data wirelessly to physicians, or into a seizure diary. “It is very difficult to obtain a good seizure diary, especially if the seizures are nocturnal,” says Loddenkemper. “We need an independent measure.”
Although his study was limited to generalized tonic-clonic seizures, a new study is underway to test the wristband’s ability to detect more subtle seizures. Loddenkemper, fellow Boston Children’s neurologist Alex Rotenberg, MD, PhD, and Bryan McLaughlin, PhD, at Draper Laboratory have a grant from CIMIT to develop a sensor that would sit under the ear, connecting wirelessly to electrodes on the scalp or implanted on the brain itself.
In a related study, Loddenkemper’s team found evidence that patterns of autonomic nervous system activity, detected by the wristband system, could identify children at heightened risk for sudden death from epilepsy – warranting especially close surveillance. “Children with severe epilepsy have an increased risk of dying during seizures,” notes Loddenkemper. “A closed-loop sensor system may enable us to prevent this.”







