
Small interfering RNAs, or siRNAs, could be great targeted treatment tools for breast and other cancers. The problem is making sure they get packaged and delivered to where they need to go. (pscf11/Flickr)
Breast cancers whose cells carry the HER2 protein are pretty tough customers. They only account for about 20 percent of all breast cancers, but they are some of the most aggressive. While targeted drugs like trastuzumab (Herceptin) and lapatinib (Tykerb) have made these tumors easier to treat, those that resist these drugs, relapse or don’t have HER2 on their cells’ surfaces can still stymie oncologists.
A molecular phenomenon called RNA interference (RNAi)—in which small pieces of RNA silence the expression of individual genes—could provide an alternative solution for breast and other cancers.
Though it was first discovered in plants, researchers have known for about a decade that small interfering RNAs (siRNAs) are active in mammals like us, and are already working on ways to harness them for shutting down genes promoting cancer and other diseases.
The problem with siRNAs for treatment, however, is making sure they get exactly where they need to go. That’s a problem that Judy Lieberman, MD, PhD, has taken a big step toward solving.
Lieberman’s laboratory in the Program in Cellular and Molecular Medicine at Boston Children’s Hospital and the Immune Disease Institute (PCMM/IDI) has worked for several years to exploit RNAi’s therapeutic potential. Last year, she published a paper showing how it could be used to develop a topical microbicide against HIV; she’s also engineered similar methods against herpes.
Now Lieberman has applied her experiences with RNAi to breast cancer. A few weeks ago, in Science Translational Medicine, she and a former fellow from her laboratory, Erwei Song, MD, PhD, reported success using siRNAs to attack tumors in a mouse model of HER2-expressing breast cancers.
“The challenge is to deliver the siRNAs to the site of the tumor without creating toxicity or inflammation in other portions of the body,” explains Lieberman. “Unpackaged or ‘naked’ siRNAs are cleared by the kidneys very quickly, and cells don’t take them up readily. There are other delivery systems, like liposomes, but they tend to collect in the liver. Which is fine for treating liver diseases but not for other areas of the body.”
Lieberman and Song (now at Sun Yat-Sen Memorial Hospital in Guangzhou, China) started with siRNAs that would turn off a gene called PLK1 (which codes for an enzyme that promotes cell division). They then made some important tweaks. First, they packaged the siRNAs in protamine, a peptide that normally shrink-wraps DNA in sperm cells. Next, they attached an antibody fragment (called an ScFv) against HER2, which essentially acts as an address label, to the packaged siRNAs.
“The protamine stabilizes the siRNAs and protects them from being broken down by enzymes in the bloodstream,” Lieberman says. “And the ScFv antibody fragment makes sure that they only get delivered to and act in HER2-positive cells.”
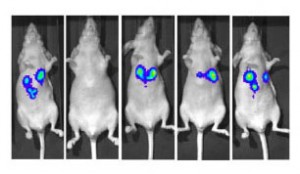
Note the second mouse from the left: it was treated with Lieberman's packaged siRNAs. And unlike its counterparts—including the one to its left, which was treated with 'naked' siRNAs—it's tumor-free.
Lieberman, Song and colleagues then injected both naked and packaged siRNAs against PLK1 into mice with HER2-positive human breast tumors. While the mice quickly cleared the naked siRNAs (their half-life in the mice’s blood was a mere six minutes), the packaged siRNAs stayed in the mice for at least 72 hours.
And the packaged siRNAs went exactly where they needed to go—right to the tumors. Once there, they penetrated the tumors’ cells and shut off PLK1, stopping tumor growth and suppressing metastasis.
Even better, the team found no evidence of inflammation or toxicity in the liver, kidneys, or bloodstream, which—along with tests showing where the siRNAs accumulated—suggested that the siRNAs were silencing PLK1 only in their intended targets.
“PLK1 is ubiquitously expressed and is needed for cells to divide,” Lieberman notes “but because we targeted the siRNAs only to HER2-expressing tumor cells, we could silence this gene with great specificity and no toxicity to other tissues.”
Lieberman sees the protamine-ScFv-siRNA combination as a potential platform for harnessing RNAi to treat a broad range of cancers and other diseases. It could even be used to deliver multiple siRNAs against multiple gene targets at once; in the same paper, she and Song showed they could deliver cocktails of siRNAs silencing different genes for a synergistic effect against the mice’s tumors.
“We have also used the platform to target lymphocytes, suggesting it could be useful against lymphomas and leukemias and as a way of countering organ rejection,” she says. “Potentially, it could be used to deliver siRNAs therapeutically to any cell for which we have a cell surface marker to target.”







