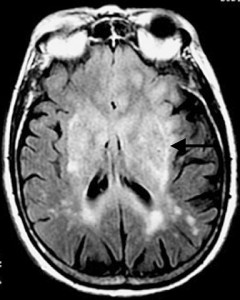
Brain tumors like the diffuse, light gray one in this MRI do a remarkably good job of hiding from the immune system. A new treatment based on gene therapy could strip their camouflage away. (Filip Em/Wikimedia Commons)
If there’s anything that tumors are good at, it’s hiding themselves. Not from things like MRIs or CT scans, mind you, but from the immune system. Since a tumor grows from what were at one time normal, healthy cells it’s still “self,” still one of the tissues that makes you you.
“Tumor cells display very subtle differences that distinguish them from healthy cells, but by and large they look the same to your immune system,” says Mark Kieran, a pediatric neuro-oncologist at the Dana-Farber/Children’s Hospital Cancer Center and Children’s Hospital’s Vascular Biology Program. “The question is: How can we unmask tumors so that the immune system can do its job?”
Researchers have worked for years on cancer vaccines aimed at getting the immune system to wake up to the presence of a tumor and turn on it. With a Phase 1 safety trial , Kieran and his colleagues, including Children’s neurosurgical oncologist Lily Goumnerova, are evaluating a different strategy for patients with hard-to-treat brain tumors called malignant gliomas: They’re giving the tumors a cold.
The team is investigating a kind of gene therapy that attacks tumors from multiple angles at once. It starts with a modified adenovirus – one of the viruses that cause the common cold – that’s surgically injected directly into the tumor. Once it’s in, it infects the tumor cells and, following its genetic programming, inserts a gene from the herpes simplex virus. The tumor cells then produce a herpes protein, which gets displayed on their surfaces. The surgery is followed with a combination of an antiviral drug like valacyclovir, , temozolomide (which, in many patients makes tumors more sensitive to radiation), and a standard radiation and chemotherapy regimen.
This treatment procedure does a few things. First, the herpes protein on the tumor cells’ surface makes them susceptible to the antiviral; the temozolomide and radiation also help the antiviral work more effectively. Second, the radiation therapy goes after any dividing blood vessel cells that the tumor might exploit to increase its oxygen supply.
Third, there’s the immunologic effect. The immune system reacts quickly to adenoviruses like the one being used in the trial, since nearly all of us have been exposed to an adenovirus at some point in our lives. In addition, dying virus-infected tumor cells release loads of tumor-associated proteins – ones the immune system doesn’t recognize as self, sending up biochemical warning flares that further draw the immune system into action.
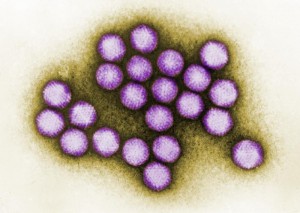
The adenovirus: Cause of the common cold, and the backbone of a possible new treatment for brain tumors. (CDC)
Add to this the fact that the herpes protein incorporated in the adenovirus is also a powerful immune stimulator, and a once hidden tumor now finds itself in an immunological environment akin to a matador waving a cape in front of a bull.
Why malignant gliomas? For starters, these are tumors with few treatment options: Even with surgery, radiation and chemotherapy, survival time is typically measured in months, rather than years. Also, glioma cells divide rapidly, unlike healthy brain cells, which stop dividing after a child is a few months old. “We’re taking advantage of the fact that glioma cells are the only nervous system cells rapidly dividing in the brain,” Kieran explains.
The Phase 1 safety trial is slated for nine patients, and Kieran’s team has already treated three. “We have seen evidence suggesting that this strategy can be effective against brain, ovarian and prostate tumors in adults,” he says. “To the best of our knowledge, this is the first time it has been tried in children with brain tumors.”
“We know we still have a lot to learn if we’re going to make it an effective treatment choice,” he continues, “but these are children who need new options for treatment, and we’re quite hopeful that this could be one of them.”