
The right inferior frontal gyrus, part of the prefrontal cortex, lights up on fMRI when children play a game requiring them to resist a natural impulse. This brain area is naturally in flux between ages 5 and 7, Sheridan has found.
Last month, the American Academy of Pediatrics released new guidelines on attention-deficit hyperactivity disorder (ADHD), lowering the minimum age at which physicians should consider drug treatment from 6 years to 4 years.
But here’s the problem. “Current behavioral criteria for ADHD are most effective only after age 8 or 9,” says Margaret Sheridan of the Laboratories of Cognitive Neuroscience at Children’s Hospital Boston. “If you use them at age 3 to 6, then you’re wrong about half the time, and the child will stop meeting the criteria by age 8.”
Little kids, especially boys, are naturally distractible, impulsive and fidgety. Some mature more slowly; some are just the youngest in their class. Many will grow out of their wild but largely age-appropriate behaviors.
But letting true ADHD fester, explaining symptoms away as “kids just being kids,” deprives children of the benefits of behavioral or pharmacologic treatment at a time when their young brains are highly responsive. They’re left to struggle in school and have negative social experiences; as adults, they are more likely to have car accidents, abuse drugs, get divorced and die at a young age.
Compounding the problem, other conditions like anxiety or autism spectrum disorders can be mistaken for ADHD, as parent callers related during a recent NPR On Point episode.
Sheridan wants to avoid these problems by finding an objective, measurable pattern of brain activity that reliably predicts ADHD in children as young as 3. Does that difference persist over time? Does it correlate with behavioral measures? Does treatment change the brain activity?
“My hope is that we could find a tool that’s relatively cheap,” Sheridan says. “We should at least make sure we’re treating the right kids.”
To date, she’s enrolled about 40 children in a study that is measuring both EEG activity and metabolic activity on functional MRI (fMRI) scans in children 3 to 7 -both typical children and children meeting research criteria for ADHD. (The fMRI studies start at age 5, when most children can hold still in the scanner). The study will ultimately enroll 200 children (for information, and to enroll a child, call Kelly Khem at 857-218-5220 or email [email protected]).
Sheridan’s broader interest is in understanding how children develop executive function: the ability to hold relevant information in mind, to inhibit actions and distraction by irrelevant information and to switch flexibly between operations or tasks. It’s critical to planning and cognitive control, both of which are impaired in ADHD.
Children naturally have a steep increase in executive function between age 5 and 7, but until now, one has tried to correlate these changes with changes in brain structure and function at such young ages.
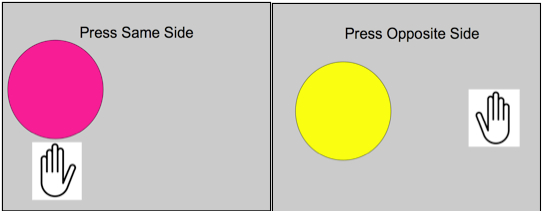
The Simon task requires children to press on the same side when they see the pink button, and the opposite side when they see the yellow button – regardless of whether the buttons are presented on the left or the right. The task forces children to overcome the innate tendency to press on the same side as the button, rather than base their response on the button color.
In a pilot study presented yesterday at the Society for Neuroscience annual meeting, Sheridan and colleagues gave 30 typically developing 5- to 10-year-olds the Simon Task, a test of inhibitory control that requires curbing an initial impulse. All children did well at this test, getting slightly better with age, but 5- to 7-year-olds used more parts of the brain during the test than did 8- to 10-year-olds. In particular, a structure known as the inferior frontal gyrus, part of the prefrontal cortex, was used less as children get older, and its gray matter actually shrank as the maturing brain pruned away unnecessary wiring.
Bottom line: The prefrontal cortex – the seat of executive function – seems to be in a period of natural flux at age 5 to 7. It certainly doesn’t seem like a time to be recklessly medicating. A better understanding of how natural development unfolds – matching kids’ performance on tests like these with their brain activity – is a necessary first step in being able to spot children who truly do have ADHD.
Once a child is diagnosed, there are highly effective behavioral interventions: computer-based training to expand executive function, and Parent-Child Interaction Therapy (PCIT), giving parents the tools to teach their children to control themselves. Sheridan and colleagues hope to conduct a trial of these interventions in young children with ADHD, and see if the clinical results are matched by changes in EEG and fMRI patterns.






