Today, a variety of approaches that attempt to either restore dystrophin or compensate for its loss are in the therapeutic pipeline.
“We’re at the point where lots of things are going into clinical trials,” says Louis Kunkel, PhD, who is credited with identifying dystrophin in 1987. “I call it the decade of therapy.”
An approach fairly far along in clinical trials is exon skipping, which tricks the cellular machinery into making dystrophin, making DMD milder. Two drugs, drisapersen (Prosensa) and eteplirsen (Sarepta Theraupeutics) accomplish this in different ways and have shown some promise in clinical trials, demonstrating increased dystrophin production and stabilized or improved muscle function.
A Phase III trial of drisapersen, reported in September 2013, failed to show improvement on a six-minute test of walking distance, but the results of extended, open-label treatment trials, presented in late April 2014 at the American Academy of Neurology annual meeting, indicate that boys who start drisapersen or eteplirsen earlier and receive it longer do better, sometimes retaining the ability to walk.
Another approach, in early clinical trials, stimulates gene activity to increase levels of utrophin, a protein that looks and acts much like dystrophin and could compensate for its absence. (Normally, utrophin is present only prenatally, replaced by dystrophin at birth.) Still other approaches use gene therapy to deliver an intact dystrophin gene; a hurdle has been finding methods that are both safe and capable of getting the gene into muscle throughout the body.
Beyond dystrophin
Not all approaches are dystrophin-based, but instead seek to address problems caused by dystrophin loss. One of these is impaired production of nitric oxide, which enables blood vessels to relax and dilate, increasing blood flow. The erectile dysfunction drugs Cialis and Viagra restore nitric oxide production, and a small study published May 7 found that they improved blood flow to DMD patients’ weakened muscles. It’s not clear, though, whether this will actually slow DMD’s progress. A phase III trial of Cialis is now enrolling patients.
Kunkel’s lab has been pursing another “dystrophin-independent” approach. Noting that loss of dystrophin sets off a cascade of inflammatory events and other insults that damage muscle, Iris Eisenberg, PhD, in the lab sought other players that could be targeted. She conducted a comprehensive scan of microRNAs, tiny bits of code that can regulate multiple genes at once, in muscle from patients with 10 different muscular disorders, including DMD. Her search turned up 185 microRNAs that were either too abundant or too scarce in diseased muscle.
Could DMD be slowed by targeting some of these microRNAs? Matthew Alexander, PhD, in Kunkel’s lab recently did a deep dive on one of them—miR-486.
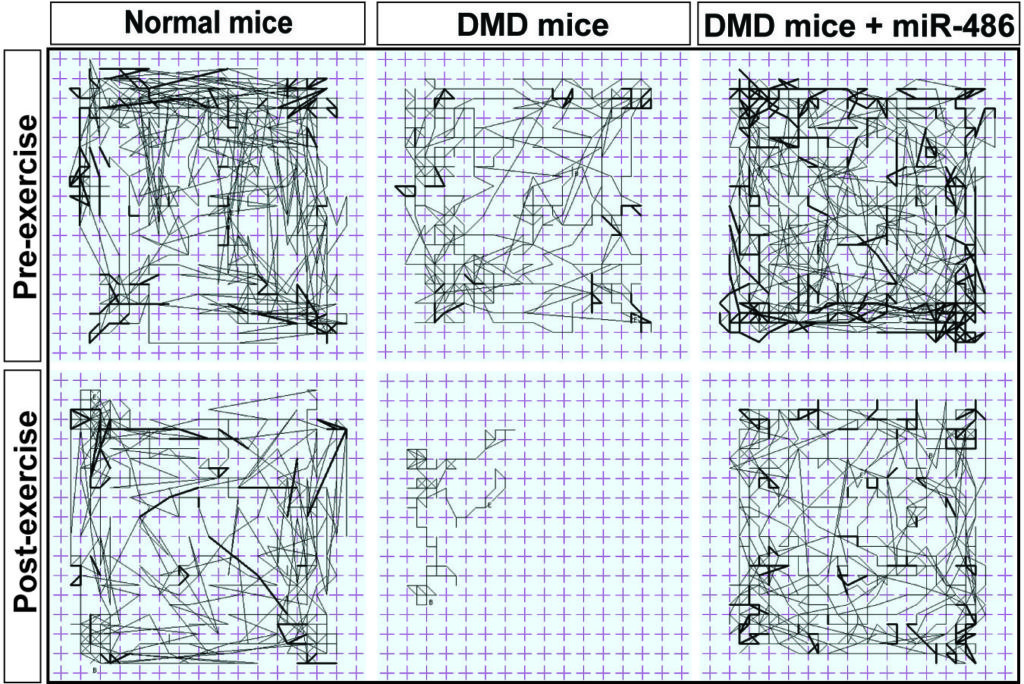
This “random walk” plot charts the movements of mice before and after exercise. Mice with DMD were clearly tuckered out from their exertions, but those able to make more miR-486 were almost as active as normal mice.
In his study, published May 1 in the Journal of Clinical Investigation, DMD mice whose muscles were manipulated into making more miR-486 had better muscle structure, physiology and performance than other DMD mice. On treadmills, they ran almost as vigorously as wild-type (normal) mice. And on the random walk plot, they were clearly less fatigued after exercise than DMD mice—and nearly as active as wild-type mice.
Alexander and colleagues then looked for the genes that miR-486 regulates, using a systematic, bioinformatics-driven approach. This led them to a molecule called DOCK3, part of a pathway that damages muscle unless miR-486 is there to suppress it. Alexander and Kunkel envision two possible therapeutic approaches: increasing levels of miR-486 or knocking down DOCK3. Kunkel hopes to begin doing drug screens to test these approaches.
While there are many approaches to DMD showing clinical promise, Kunkel believes it’s important to continue the discovery process, one he’s been engaged in for more than 30 years.
“There will not be one unique therapy,” he predicts. “It’s always going to be a combination. None of these are curative, so it’s never going to be a single entity, but a cocktail of different approaches.”







